Black Spots on Teeth That Aren’t Cavities: An In-Depth Guide to Causes, Treatment, Prevention, and Broader Community Health Implications

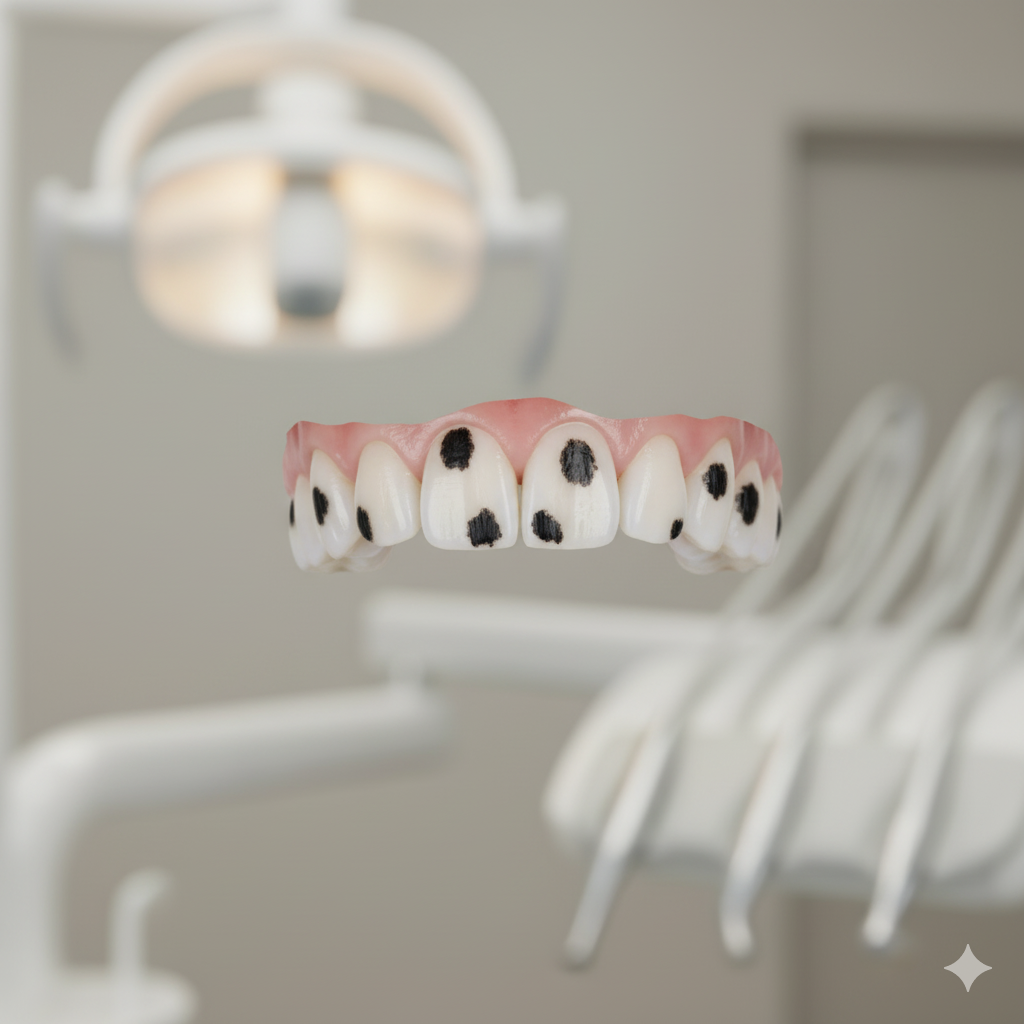
The appearance of black spots on teeth that aren’t cavities is a surprisingly common concern for people across all age groups. Tooth discoloration often triggers anxiety because many assume that any dark mark represents tooth decay or deeper damage. However, dentistry has long recognized that not all dark spots signify cavities. In reality, these spots may stem from a variety of harmless, reversible, or simply cosmetic reasons. Understanding their causes, implications, and treatment options empowers individuals to make informed choices while reducing unnecessary fear. Additionally, exploring the social and systemic factors behind oral health—such as regional impact, policy frameworks, rural development, women empowerment schemes, and social welfare initiatives—helps us see how oral hygiene is influenced by community-level planning, not just personal habits.
This comprehensive guide explains every major cause behind black spots on teeth that aren’t cavities, how dentists distinguish them from decay, and what modern treatment options look like. It goes beyond the surface to explore how oral health programs are implemented across regions, how state-wise benefits help bridge dental care gaps, and why inclusive policy development matters for long-term outcomes. It also highlights success stories, real-world examples, challenges in implementation, comparisons with other public health frameworks, and future prospects for improving dental wellness for all.
Understanding the Nature of Black Spots on Teeth That Aren’t Cavities
Dentists commonly encounter patients who notice small dark marks during brushing or chewing. The immediate assumption that these marks are cavities leads to panic, often unnecessarily. Cavities themselves result from bacterial activity that erodes the enamel and dentin. However, black spots on teeth that aren’t cavities can come from pigmentation, mineral deposits, environmental factors, or benign surface stains.
The history of dental science shows that early civilizations also grappled with tooth discoloration. Ancient Egyptian papyri describe herbal treatments used to whiten teeth, while Roman texts illustrate the use of pumice powder. These early attempts indirectly recognized that discoloration has many causes. As dentistry evolved through the 18th and 19th centuries with scientific classification of enamel and dentin structure, specialists began identifying distinctions between stains, mineral streaks, and true decay. Modern diagnostics, including bitewing radiographs and laser fluorescence tools, now allow dentists to differentiate between discolored enamel and cavity lesions with high accuracy.
Understanding these distinctions is essential because treatment varies widely. While cavities require restorative work, non-carious discoloration may only need cosmetic polishing, dietary modifications, or preventive care.
Common Causes of Black Spots on Teeth That Aren’t Cavities
Extrinsic Stains from Food, Drinks, and Tobacco
One of the most frequent causes of black spots on teeth that aren’t cavities is external staining. Dark beverages like coffee, tea, red wine, and cola contain chromogens that bond to enamel. Over time, these pigments settle in microscopic grooves, forming stubborn marks. Tobacco, both smoked and chewed, leaves tar-like deposits that appear as black streaks or dots. These stains are surface-level and reversible with professional cleaning or whitening.
Calculus and Tartar Buildup
When plaque remains on teeth for extended periods, it calcifies into tartar, which can appear yellow, brown, or black depending on its mineral content. Subgingival tartar (below the gumline) often appears darker due to trapped pigments and bacterial byproducts. Some individuals naturally accumulate more tartar due to saliva composition, medication, or dietary factors.
Developmental Enamel Defects
Developmental conditions such as enamel hypoplasia or fluorosis may result in pigmentation patches. These defects form during childhood when teeth are still mineralizing. The affected enamel becomes porous and can trap pigments. Although structurally intact, these areas look like black spots on teeth that aren’t cavities.
Metallic Exposure and Environmental Factors
Certain metals—including iron, manganese, and copper—can stain teeth upon contact. In regions with high mineral content in groundwater, residents may develop distinct spotting patterns. This links dental health with regional impact and environmental conditions. State-wise water quality initiatives and rural development programs sometimes target this issue, recognizing that oral and general health share common determinants.
Chromogenic Bacteria
Some bacteria produce pigmented byproducts. In children especially, a particular strain of bacteria is known to create dark lines along the gumline. These look alarming but are harmless and tend to diminish over time. Regular cleaning easily removes these deposits.
Old Dental Restorations
Silver amalgam fillings occasionally release corrosion products that cause grayish-black staining on adjacent enamel. These marks do not indicate renewed decay but may cause cosmetic concern.
Dietary and Behavioral Patterns
Habitual consumption of certain foods—like betel nut, often used in South Asian regions—causes deep, persistent stains. Social welfare initiatives promoting oral hygiene frequently include awareness campaigns against such habits.
Differentiating Between Cavities and Non-Cavity Spots
Although patients may confuse the two, dentists rely on key diagnostic differences:
● Cavities usually appear as soft, chalky, or rough areas when probed.
● Non-cavity black spots feel hard and smooth.
● Radiographs of cavities show shadows extending into dentin; stains remain superficial.
● Spot patterns also differ: cavity lesions cluster in high-risk zones like pits and fissures, whereas non-cavity spots may appear randomly.
Understanding this distinction prevents unnecessary procedures and helps patients feel reassured. It also encourages early intervention for actual caries risk.
Regional Impact and Community-Level Oral Health Implementation
Oral health disparities often reflect broader socio-economic conditions. When communities lack dental services, awareness, or preventive resources, issues like black spots on teeth that aren’t cavities become difficult to address. Many regions, especially rural districts, face limited access to qualified dentists, leading to delays in diagnosis.
Community dentistry programs have shown that preventive action—fluoride varnish application, sealant programs, school health drives, and outreach screenings—dramatically improve oral health outcomes. In many states, public health frameworks incorporate oral hygiene into overall wellness programs. The regional impact becomes visible when policy interventions reduce avoidable discoloration and disease.
Local governments often integrate oral health into rural development agendas, recognizing the link between nutrition, sanitation, drinking water, and dental appearance. Awareness efforts that target early childhood dental hygiene—such as discouraging sugary snacks—help reduce both stains and caries development.
Policy Framework Supporting Oral Health and Hygiene Awareness
A robust policy framework can reduce the prevalence of both cavities and non-cavity discoloration. Governments sometimes include dental health in larger social welfare initiatives. These may cover school dental camps, subsidized checkups, training programs for community health workers, and safe drinking water schemes.
Policy alignment with global standards, such as WHO recommendations for fluoride control and sugar consumption thresholds, strengthens these efforts. In regions where high fluoride levels cause enamel staining, state-level water purification projects become essential. Policies supporting dental infrastructures—mobile clinics, tele-dentistry, and digital health records—help extend services to underserved populations.
This systemic approach reduces not only disease burden but also the psychological stress associated with dental discoloration, including concerns over black spots on teeth that aren’t cavities.
State-Wise Benefits and Programs for Dental Care Access
States with strong public health investment often provide incentives and coverage for dental screenings. Some regions implement free annual check-ups for schoolchildren, enabling early detection of both cavities and non-cavity spots. Others subsidize community fluoride testing to prevent excessive exposure, which contributes to enamel staining.
Women empowerment schemes integrated into healthcare often train women health workers to educate local households about oral hygiene. Their outreach greatly benefits rural families who may not regularly visit clinics. This approach acknowledges that dental health improvement goes hand-in-hand with broader empowerment and education.
By understanding state-wise benefits, one can appreciate how local initiatives reduce the occurrence of untreated discoloration and improve community awareness.
The Role of Social Welfare Initiatives in Dental Health
From subsidized toothpaste distribution to widespread public messaging, social welfare programs play a substantial role in oral health. Some initiatives focus on child nutrition programs, which indirectly improve dental health by reducing sugar dependence. Others include sanitation and clean water projects that curb mineral-induced staining.
When oral health becomes part of a social welfare ecosystem, individuals are more likely to seek professional care early, preventing misinterpretations of black spots on teeth that aren’t cavities. This holistic approach highlights the importance of integrating dentistry into society’s broader development goals.
Women Empowerment and Oral Health Advocacy
In many communities, women serve as primary caregivers for children. Women empowerment schemes strengthen health education by supporting mothers with resources to improve family hygiene. Training sessions often include oral care modules—demonstrating proper brushing, identifying signs of dental trouble, and understanding harmless discolorations.
Women-led self-help groups sometimes collaborate with local health departments to distribute dental hygiene kits. These programs indirectly reduce fear and misconceptions about tooth discoloration and ensure children’s early exposure to correct oral care.
Challenges in Addressing Non-Cavity Tooth Discoloration
Despite advancements, several challenges remain:
Limited Access to Dental Professionals
Many rural areas lack dentists, leading to self-diagnosis or neglect. People often mistake benign stains for cavities, causing unnecessary anxiety.
Economic Barriers
Even when services exist, costs may prevent regular cleaning. Cosmetic treatments like whitening or enamel microabrasion remain unaffordable for many.
Cultural Beliefs and Stigma
Some communities view tooth discoloration as a sign of poor hygiene or disease. This stigma discourages people from seeking help.
Lack of Awareness
People often cannot distinguish between cavities and harmless discoloration. Misconceptions spread quickly, especially in areas with limited dental education.
Inconsistent Policy Implementation
While policy frameworks exist, uneven execution across states or districts can hinder progress. Monitoring and evaluation remain essential to ensure equitable benefits.
Success Stories and Real-World Impact
Many states and regions have demonstrated measurable success through well-planned oral health programs:
School Fluoride Varnish Programs
Introduced in several rural regions, these programs cut caries rates significantly. Even though the focus is decay prevention, children also benefit from professional oversight detecting non-cavity black spots early.
Mobile Dental Clinics
These clinics travel to remote villages offering scaling, polishing, and stain removal. Their service helps address black spots on teeth that aren’t cavities and other concerns without requiring travel.
Women-Led Community Health Drives
Women empowerment schemes have resulted in successful grassroots dental awareness campaigns. Mothers trained in hygiene education have improved children’s brushing habits and reduced stain-related complaints.
Water Quality Improvement Projects
State-wide water testing and purification initiatives have reduced enamel fluorosis severity in mineral-heavy regions. As fluoride-induced discoloration declines, residents experience improved confidence and reduced stigma.
Comparison with Other Public Health Schemes
Dental health initiatives share similarities with broader public programs. For example:
● Like nutritional schemes, dental programs depend on consistent community engagement.
● Like maternal health programs, oral hygiene efforts benefit from women empowerment initiatives.
● Like sanitation projects, fluoride control and water quality improvement address environmental determinants of health.
● Like child immunization campaigns, school dental screenings rely on large-scale coordination.
However, dental programs often receive less funding and attention. Unlike high-profile public health issues, oral health concerns—such as black spots on teeth that aren’t cavities—are often overlooked. Strengthening dental infrastructure requires policymakers to treat oral hygiene as integral to overall public health.
Treatment Options for Black Spots on Teeth That Aren’t Cavities
Several professional and home-based treatments can address non-cavity discoloration:
Professional Cleaning
Scaling and polishing remove surface-level stains and tartar. This is the most common solution and provides immediate cosmetic improvement.
Air Polishing or Prophy Jet
Dentists use fine powders to gently remove pigmentation without damaging enamel.
Enamel Microabrasion
A minimally invasive technique that removes superficial enamel irregularities causing dark spots.
Whitening Procedures
LED, laser, or chemical whitening lifts deeper stains. Whitening is safe when performed professionally.
Resin Infiltration
For developmental defects, resin infiltration blends uneven coloration.
Addressing Underlying Causes
Treatment may involve switching water sources, avoiding staining foods, quitting tobacco, or improving brushing technique.
Understanding what caused the black spots on teeth that aren’t cavities ensures long-term prevention.
Prevention Strategies: Individual and Community-Level Approaches
Daily Oral Care
Twice-daily brushing, flossing, and periodic use of whitening toothpaste help control pigments and plaque.
Diet Management
Reducing intake of chromogenic foods and beverages prevents new stains.
Water Quality Awareness
In areas with high fluoride or mineral levels, filter usage or community water programs help protect enamel.
Regular Dental Visits
Routine checkups help distinguish cavities from harmless discoloration.
Community Health Programs
State-level and rural development initiatives further reinforce awareness by integrating dental care into schools, public health centers, and women empowerment schemes.
Future Prospects for Managing Black Spots and Improving Oral Health
Looking ahead, several exciting developments promise better oral health outcomes:
Technological Advancements
AI-assisted diagnostics will improve early detection and differentiation of cavity vs. non-cavity discoloration. Portable dental devices will expand services to remote regions.
Policy Evolution
Governments increasingly recognize oral health as essential. Future frameworks may provide subsidies for whitening treatments or regular dental scaling, reducing the prevalence of stains and discoloration.
Expansion of Rural Development and Women Empowerment Programs
Training more women health workers ensures deeper penetration of dental awareness across rural communities.
Integration into Telehealth Platforms
Virtual dental consultations will help individuals understand whether black spots on teeth that aren’t cavities require treatment or not—reducing fear and unnecessary clinic visits.
Strengthening Social Welfare Systems
Holistic welfare schemes combining nutrition, sanitation, water quality, and oral hygiene will further improve community dental outcomes.
The future points toward inclusive, accessible, technology-driven dental care.
FAQs
What are the most common causes of black spots on teeth that aren’t cavities?
They typically come from stains, tartar buildup, water minerals, old restorations, or harmless bacterial pigments.
How can I know if the black spot is a cavity or just a stain?
A dentist can tell by examining texture, hardness, and radiographs. Stains remain superficial and smooth, while cavities create soft or rough areas.
Can black spots on teeth that aren’t cavities be removed at home?
Mild staining can improve with whitening toothpaste, but tartar or deeper stains need professional cleaning.
Are these black spots harmful?
Most non-cavity spots are harmless. However, professional evaluation ensures no underlying issue is missed.
Do children get black spots that aren’t cavities?
Yes. Chromogenic bacteria and enamel defects often cause harmless spots in children.
Can water quality cause tooth discoloration?
Yes. High fluoride or mineral levels can create dark patches or streaks.
How do dentists treat black spots on teeth that aren’t cavities?
Treatments range from scaling, polishing, and whitening to microabrasion and resin infiltration, depending on the cause.