Understanding the TMJ Surgery Cost
Temporomandibular joint disorders (TMD) affect the hinge connecting the jawbone to the skull, making everyday functions such as chewing, speaking or even yawning a painful ordeal. When conservative treatments fail, surgical options may be considered — and the question patients most commonly ask is: what is the TMJ surgery cost? In this article we explore this question in depth. We’ll examine historical context, objective reasons for surgery, implementation of care, state-wise or regional variation, comparative policy/insurance frameworks, success stories, challenges, and future prospects — so you have a well-informed perspective on TMJ surgery cost.

A Brief History and Background of TMJ Disorders and Surgery
The term “TMJ” refers to the temporomandibular joint itself — the joint connecting the mandible (lower jaw) to the temporal bone of the skull. Over time, recognition of disorders affecting this joint (sometimes grouped under TMD) has evolved. Initially thought of as dental issues (occlusion, bite misalignment, bruxism), the understanding gradually expanded to include muscular, skeletal, neurological and even psychosocial contributors.
Surgical intervention in TMJ disorders emerged as a last‐resort option after non‐invasive treatments showed limited effectiveness. Historically, early surgeries for the joint were somewhat experimental and carried significant risk; over time, techniques improved — arthrocentesis (flushing of the joint space), arthroscopy, open-joint repair, and even joint replacement became possible.
As clinical awareness grew, so did the conversation about cost. Unlike more standardised surgeries (e.g., hip or knee replacement), TMJ surgeries lacked consistent pricing, standard protocols, or universal insurance coverage. This variability has a direct bearing on TMJ surgery cost. According to the TMJ Association, there is no standardised cost for TMJ treatments; fees vary by provider, location and the details of the procedure.
In short: TMJ surgery cost reflects a procedure rooted in complex anatomy, variable indications, evolving techniques and inconsistent policy/regulation — all of which contribute to wide cost ranges.
What is the Objective of TMJ Surgery?
Before discussing cost, it’s important to understand what surgery aims to achieve. The objectives of TMJ surgery are:
-
To relieve pain and dysfunction of the jaw joint, especially when non-surgical therapies (splints, physical therapy, medications) have failed
-
To restore range of motion, reduce joint noises (clicking, popping), and improve chewing or speaking function
-
To correct anatomical or structural deficits: damaged cartilage, degenerative changes, ankylosis (fusion), displaced disc or condyle, or joint replacement where necessary
-
To improve quality of life: alleviating chronic headache or ear-ache symptoms that stem from TMJ dysfunction
-
Ultimately, to provide a durable solution rather than repeatedly tinkering with conservative therapy
Given these objectives, TMJ surgery cost must be viewed as an investment in potentially long-term relief for individuals whose TMD has become disabling. Decision-makers (patients, families, insurers) must weigh cost against benefits, alternative treatments and risk.
Implementation: Types of TMJ Surgery and Their Cost Components
When we talk about “TMJ surgery cost”, it’s not a single number. Rather, the cost depends on which procedure is performed, the complexity of the case, geographic region, the surgeon’s expertise, facility and auxiliary costs (imaging, anaesthesia, post-op care). Below are the main types of TMJ surgery and how they influence cost.
1. Arthrocentesis
A minimally invasive flushing of the joint to remove debris or inflammatory mediators. According to one source, costs may begin at a few hundred dollars. Although resources differ, this is the entry level in the surgical spectrum.
2. Arthroscopy
A keyhole approach using a small incision and camera, sometimes repairing or repositioning components of the joint. Costs tend to be higher. One clinic noted arthroscopy “$5,000 or more per joint”. Because it requires general anaesthesia, specialised equipment, and a surgeon trained in TMJ arthroscopy, the cost rises.
3. Open-Joint Surgery (Arthrotomy / Arthroplasty)
Here the joint is fully exposed, repairs or reconstructions occur (e.g., disc repositioning, condyle reshaping). Costs range widely: from $5,000 on the low end to tens of thousands on the high end, depending on complexity.
4. TMJ Replacement
If the joint is severely damaged, a prosthetic joint may be used or bone grafting performed. This is the highest cost category. For example, one resource shows cost from $40,000 to $70,000.
Key Cost-Influencing Components
-
Surgeon’s expertise: More specialised surgeons will charge higher fees.
-
Facility and anaesthesia fees: Use of hospital operating theatre, recovery room, general anaesthesia, imaging, overnight stay all add cost.
-
Geographic location: Costs vary significantly depending on region, urban vs rural, cost of living.
-
Extent of procedure: Complexity of disease, need for grafts or replacement, bilateral vs unilateral joint, or additional orthodontic work increases cost.
-
Pre- and post-operative care: Pre-op imaging (MRI, CT), diagnostic tests, post-op physical therapy, follow-up visits, night guards.
-
Insurance coverage and policy framework: If the surgical cost is considered medically necessary or cosmetic may affect coverage and thus out-of-pocket cost.
As a summary: the term “TMJ surgery cost” must be understood as a spectrum — maybe from a few thousand dollars to tens of thousands — depending on lots of factors.
TMJ Surgery Cost: Regional and State-Wise Variations
While many cost estimates are derived from the United States context, the principle that cost varies by region holds globally. For example, in South Florida (Hallandale area) the breakdown shows arthrocentesis at ~$3,000-$5,000, arthroscopy at ~$10,000-$20,000, open-joint surgery up to $50,000.
In New York City, one blog gives ranges: minimally invasive $2,000–$20,000, open-joint $10,000–$50,000.
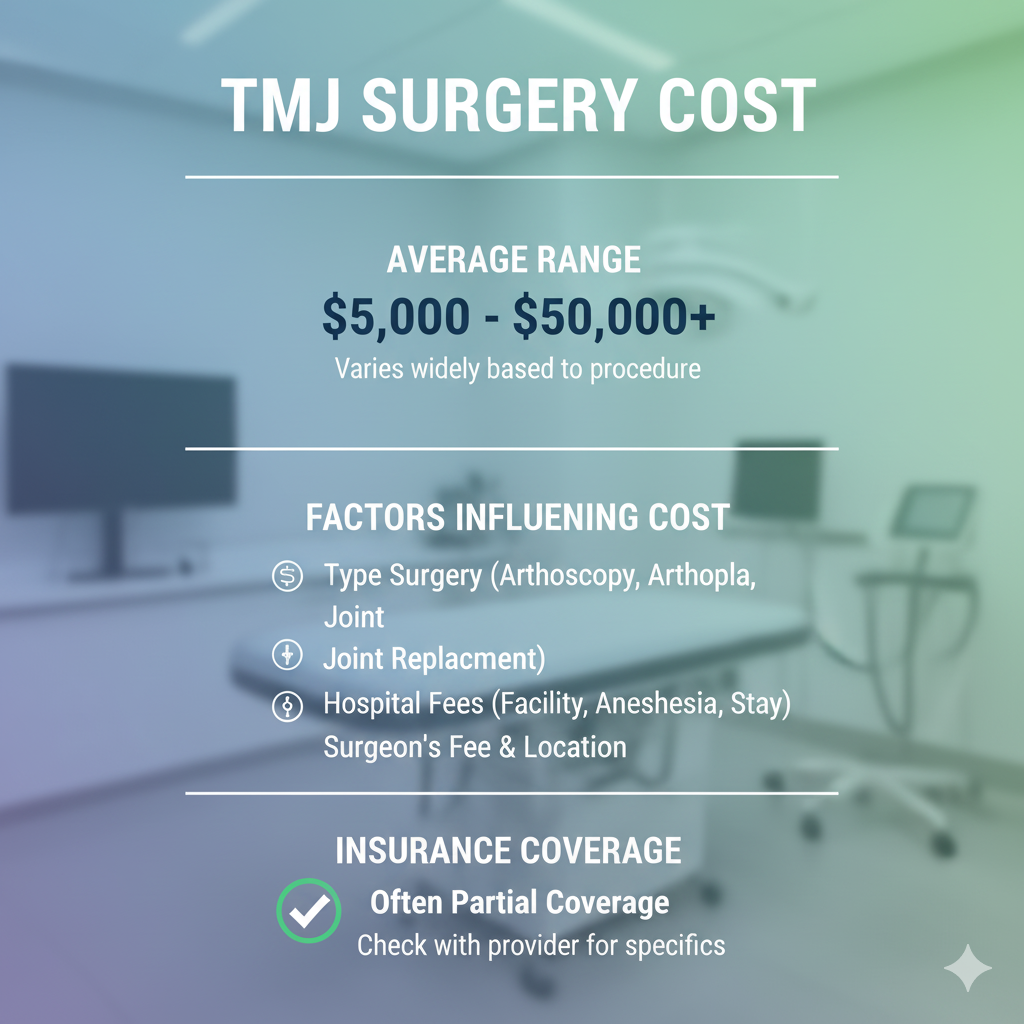
A broader American-based practice shows $5,000–$50,000 as typical range for TMJ surgery.
Why do state/region differences exist?
-
Higher cost of living and medical overhead in metropolitan states increases fees.
-
Local surgeon availability and specialisation: urban centres with many TMJ-specialists may have higher demand and higher cost.
-
Insurance regulation and mandated coverage vary by state — some states may require certain coverage for TMD, others not.
-
Competition and clinic options: in rural or less affluent states, fewer specialised surgeons may mean higher cost or longer wait.
-
Ancillary costs such as travel, lodging (if one travels to specialised centre) may add to real cost though not always included in “surgery cost” headline.
What this means for patients
When discussing TMJ surgery cost, a patient living in a small town might be quoted a significantly different figure than someone in a major urban centre. Also, outside the United States, the cost may differ further — lower due to lower overhead, or higher due to import of specialised prostheses or fewer specialists. Although this article uses US-based data, the principle of regional cost variation holds.
Policy Framework, Insurance and Coverage Considerations
One of the trickiest aspects of TMJ surgery cost is the question of who pays, or how much the patient pays out of pocket. Insurance coverage for TMD and TMJ surgery is inconsistent. The TMJ Association notes that many policies exclude TMJ treatment or limit coverage significantly.
Key policy & insurance issues
-
Medical vs dental classification: Many insurers treat TMJ disorders as dental rather than medical, thus limiting coverage or excluding entirely.
-
Evidence of effectiveness: Some insurers argue there is insufficient evidence for surgery effectiveness, reducing coverage willingness.
-
State mandates: Some states may mandate coverage for TMD but many do not. Insurance plan coverage thus varies by state.
-
Pre-authorisation and documentation: To qualify for coverage, patients must often show failed conservative therapy, imaging evidence, functional impairment, surgeon recommendation.
-
Out-of-pocket payment / financing: Because coverage is not guaranteed, patients often face large out-of-pocket costs or must rely on payment plans, third-party financing, health credit cards.
Implications for TMJ surgery cost
-
A nominal cost of, say, $30,000 for open-joint TMJ surgery may translate into much higher actual cost for a patient if insurance covers only a fraction, or not at all.
-
Patients must factor in not just the surgical fee, but imaging, diagnostics, post-op therapy, devices (night guards), time off work — all of which increase the effective cost.
-
For rural patients or state residents where specialist availability is low, the travel and lodging cost may add significantly to out-of-pocket expense even if the “headline” surgical cost is similar.
-
Given the policy/coverage uncertainty, getting multiple surgeon opinions, detailed cost breakdowns, and insurance pre-authorisation is prudent.
Thus, when evaluating TMJ surgery cost, patients should look beyond the surgeon’s fee to the total cost of treatment and coverage risk.
Success Stories and Impact Analysis
Given the expense and complexity of TMJ surgery, it’s helpful to consider real-world outcomes and success stories. While rigorous large-scale long-term studies are limited, many patients report significant improvement in quality of life.
Case examples
One source notes that for patients in whom non-surgical options have failed, TMJ surgery (arthroscopy or open-joint) may achieve success rates of 80-90%.
While detailed state-wise impact data is scarce, anecdotal reports from major centres indicate that patients who continue with debilitating jaw pain, ear pain, headaches and clicking — after countless splints and therapy — often consider surgery as the turning point.
Broader impact
-
Functional improvement: Post-surgery patients frequently regain the ability to chew properly, speak comfortably, and reduce pain episodes.
-
Quality of life: Reduced headache, ear-ache, sleep disturbance (which often accompany TMD) improve daily functioning and productivity.
-
Cost-benefit over time: While upfront TMJ surgery cost is high, some argue that repeated failed conservative treatments (splints, physical therapy, medications) themselves incur ongoing cost and lost productivity. If surgery succeeds, overall cost over five to ten years may be more favourable.
-
Regional access: In states with advanced TMJ centres, patients may travel, creating “centres of excellence” effect; rural or underserved states may have fewer high-level specialists, making access to surgery and post-operative care more difficult and increasing effective cost (travel, lodging, time off work).
Challenges in TMJ Surgery: Why the Cost Remains so Variable
Despite advancements, multiple challenges keep TMJ surgery cost wide-ranging and the decision complex.
1. Diagnostic ambiguity and limited evidence base
Because TMJ disorders are multifactorial (muscle, joint, bite, posture, psychogenic elements), some surgeries may have variable outcomes. Insurance companies often cite “lack of sufficient high-quality evidence” as reason for limited coverage. When outcome uncertainty exists, cost risks rise for the patient.
2. Specialist availability and training
Not all oral & maxillofacial surgeons or dental specialists focus on TMJ disorders. The more experienced the surgeon and the more complex the procedure, the higher the cost tends to be. For many patients in less urban regions, access may require travel to specialists, thereby increasing total cost (surgery + travel + lodging + lost time).
3. Post-operative care and maintenance
Surgery is rarely the entire solution — follow-up physical therapy, night guards, check-ups, dietary modifications are often necessary. These ongoing costs can add substantially to the “true” cost of TMJ surgery over time.
4. Insurance and policy inconsistency
As discussed earlier, whether TMJ surgery cost is covered or partly covered depends heavily on policy classification, state regulation, and documentation. The uncertainty increases financial risk to patients.
5. Regional economic disparities
Costs reflect local economics — surgical fees, hospital charges, living cost, surgeon demand. Patients in lower-income or rural areas may face fewer choices or longer travel which elevates indirect cost; conversely, patients in high-cost metropolitan areas may pay more for similar procedures.
6. Complex cases and comorbidities
Patients with severe joint degeneration, previous failed surgeries, bilateral condition, associated orthodontics or sleep-apnea problems may require multi-stage interventions, raising the TMJ surgery cost significantly (> $50,000 in some cases).
Because of these challenges the patient considering TMJ surgery must plan carefully, ask for detailed breakdowns, consider risks and alternatives, and understand the full financial commitment.
Comparison with Alternative Schemes and Treatments
To truly evaluate TMJ surgery cost, it helps to compare surgical approaches with non-surgical alternatives, and to understand when each is appropriate.
Conservative treatment alternatives
-
Splints/Night guards: Custom devices to reduce clenching/grinding, relieve pressure on the joint. Cost is modest ($200-$600 or so) in many cases.
-
Physical therapy, posture correction, muscle relaxation: Designed to relieve muscle-based TMD. Cost varies but much less than surgery.
-
Medications (analgesics, muscle relaxants): Low cost relative to surgery, but often temporary relief.
-
Orthodontics or bite correction: May be moderately priced, but combination therapies may still lead to elevated cost.
-
Minimally invasive surgical options: As noted, procedures like arthrocentesis or simple arthroscopy fall in mid-cost zone ($3,000 to $20,000) and sometimes succeed without full open-joint repair.
Cost-benefit comparison
-
Short term: Non-surgical options cost less upfront, but may require ongoing treatment, multiple visits, devices, lost productivity if pain continues.
-
Long term: If conservative methods fail and surgery succeeds, the higher upfront TMJ surgery cost may be offset by improved function, fewer visits, fewer interventions, less lost productivity.
-
Risk vs reward: Surgery carries more risk, higher cost, longer recovery; conservative treatments are lower risk and lower cost, but may not resolve the underlying structural issue.
Decision-making framework
When considering TMJ surgery cost vs alternatives:
-
Has conservative therapy failed (splints, therapy)?
-
How much is pain/function impacting quality of life?
-
What are the estimated costs of continued conservative care over 5-10 years?
-
What are the likely outcomes of surgery in your case (based on evidence, surgeon’s experience)?
-
What financing/insurance options are available for surgery?
-
What are the indirect costs (lost work, travel, lodging, recovery time)?
Thus, comparing costs is not simply comparing numbers — it’s analysing outcomes, longevity, risk, quality of life and financial burden over time.
Future Prospects: Where TMJ Surgery Cost Might Be Headed
Looking ahead, several trends may influence TMJ surgery cost, access and outcomes.
Advances in surgical technique and technology
As arthroscopic tools improve, imaging (MRI, CT) becomes more precise, and prosthetic joint designs evolve, there is potential to reduce recovery time, complication rates and thereby reduce cost over time. For example, better minimally invasive techniques might lower the cost band for certain surgeries.
Increased evidence base and policy change
Should more high-quality clinical trials demonstrate long-term benefit of certain TMJ surgeries, insurers may broaden coverage, reducing patient out-of-pocket cost. This could standardise pricing more across regions, reducing extreme variations in TMJ surgery cost.
Telehealth and multidisciplinary care
Remote pre-operative assessments, physical therapy via telehealth, and virtual follow-up may reduce adjunct costs associated with surgery (travel, lodging). Lowering these indirect costs could reduce the “true” TMJ surgery cost from the patient’s perspective.
Geographic and global disparities
As globalisation of healthcare continues, some patients may seek TMJ surgery abroad (medical tourism) where cost is lower, but this introduces issues of follow-up care, travel risk, quality assurance. Such alternatives might pressure local providers to reconsider pricing. Nonetheless, quality, safety and regulatory frameworks must be factored.
Preventive emphasis and early intervention
If earlier detection of TMD and more effective non-surgical management become standard, fewer patients may reach the point of needing expensive surgery — which might reduce demand and thus downward pressure on TMJ surgery cost.
Patient-financing and payment models
With increasing awareness of high cost of TMJ surgery, more clinics may offer payment plans, bundled cost packages (surgery + post care), or discounts for upfront cash payment — making the cost burden more manageable for patients. Some may offer outcome-based pricing or lower cost options for select indications.
Practical Steps for Patients Considering TMJ Surgery Cost
If you or someone you know is considering TMJ surgery, here are actionable steps to assess the cost and plan accordingly:
-
Obtain multiple consultations: See at least one TMJ-specialist (oral & maxillofacial surgeon or TMJ-focused dentist) and ask for a detailed breakdown of procedure, cost estimate, recovery, alternatives, risks and expected outcome.
-
Ask for itemised cost estimate: Surgeon’s fee, facility fee, anaesthesia fee, imaging/diagnostic cost, post-operative therapy, device costs (e.g., night guards), travel/lodging if required.
-
Check insurance coverage: Determine if TMJ surgery is covered, what the policy covers (surgeon, hospital, devices), what documentation is needed (failed conservative therapy, imaging, functional impairment).
-
Factor in indirect costs: Time off work, travel, lodging (if you must go to a specialist centre), post-op diet changes, therapy sessions, follow-up visits — these may add significantly.
-
Compare cost vs long-term benefit: Estimate cost of ongoing conservative therapy if surgery is delayed — multiple splint replacements, therapy sessions, lost productivity.
-
Review surgeon’s experience and outcomes: A lower cost surgeon with fewer TMJ-specific cases may carry higher risk of needing revision surgery — revision increases cost dramatically. Paying more now might save cost later.
-
Ask about payment options: Some clinics offer payment plans, interest-free financing, or discounts for upfront payment.
-
Review recovery timeline: Understand when you can return to work, what restrictions apply, how long therapy will continue — downtime is part of cost.
-
Plan for post-operative device costs: In many cases, even after surgery you’ll need night guards or maintenance therapy. These should be included in your cost budget.
-
Stay realistic and informed: Understand that “lowest cost” may not always provide best outcome. Given the variability in TMJ surgery cost, ensure you’re not sacrificing quality for cost alone.
Summary: What Patients Really Pay and Why
Putting all of this together, what can you expect when you ask “How much is TMJ surgery cost”? Here’s a rough summarisation:
-
For minimally invasive procedures (arthrocentesis or small arthroscopy) costs may begin in the range of $3,000 – $10,000 (USD), depending on location.
-
For more common arthroscopy or moderate open-joint repair, costs may range $10,000 – $30,000.
-
For advanced open-joint repair, bilateral surgery, prosthetic joint replacement, costs may reach $40,000 – $70,000 or more.
-
In some stated sources, the top end of cost may exceed $50,000.
-
Insurance may not cover the full cost (or any cost) — meaning out-of-pocket may be substantial.
-
Total cost to the patient should include not just surgical fee but diagnostics, ancillary care, post-op therapy, devices, travel/time off work.
-
Regional/state variation is large; metropolitan vs rural context matters a lot.
-
Because of the wide variability, only an individual consultation with a specialist in your region can yield a reliable estimate of your TMJ surgery cost.
Keep in mind: the high cost may be justified when the alternative is continuing pain, dysfunction, lost quality of life, repeated failed therapies, and ongoing indirect costs. The decision is not simply “how much does it cost” but “what is the value of relief and restored function”.
FAQs about TMJ Surgery Cost
1. How can I estimate the cost of TMJ surgery in my region?
First book a consultation with a TMJ-specialist or oral & maxillofacial surgeon in your area. Ask for a full breakdown: surgeon fee, facility/operating room cost, anaesthesia, imaging, follow-up, devices (night guard), travel/time off work. Also ask how many similar cases they perform per year. Check your insurance policy for TMJ coverage. Ask about payment plans.
2. Does insurance normally cover TMJ surgery cost?
Coverage is inconsistent. Many dental plans exclude TMJ, or treat it as a dental rather than a medical issue. Some medical insurance covers it if it meets criteria (failed conservative therapy, functional impairment, structural damage), but many plans have exclusions. The patient should verify coverage with insurer and obtain pre-authorisation where possible.
3. Why does TMJ surgery cost vary so much between patients?
The wide variation stems from: types of surgery (arthrocentesis vs open-joint vs replacement), surgeon’s experience, facility/hospital vs outpatient centre, geographic location (cost of living, specialist demand), extent of the jaw/joint damage, bilateral vs unilateral surgery, pre-operative and post-operative needs, travel/time off work. All these factors expand the cost range.
4. Is the high cost of TMJ surgery always worth it?
It depends on the individual. For patients whose quality of life is severely affected, where non-surgical methods have failed, and the surgery is performed by an experienced specialist, the high cost can be justified by improved function and quality of life. Conversely, for mild cases where conservative therapy is still viable, the cost may not be warranted. Discuss outcome statistics, risks, and alternatives thoroughly.
5. What hidden costs should I anticipate when considering TMJ surgery cost?
Beyond the headline surgical fee, anticipate: pre-operative imaging (MRI, CT), diagnostics, initial consultations, possible travel/lodging if you need a specialist centre, time off work, post-operative physical therapy, night guards or splints after surgery, follow-up visits, dietary modifications/restricted food cost, possible revision surgery (if the first is unsuccessful). These can cumulatively add significantly.
6. Are there ways to reduce the TMJ surgery cost?
Yes. Some strategies include: Choose a surgeon who is experienced and may offer bundle pricing or cash-discount option; schedule surgery in a season or facility where fees are lower; consider outpatient surgical centres rather than large hospitals (if appropriate); check for payment or financing plans; ask about follow-up therapy packages; ask if simplified procedure is possible (if clinically appropriate) rather than full open-joint replacement; verify insurance coverage thoroughly and ensure prior authorisation.
7. If I live in a rural or less-specialised region, what should I consider in relation to TMJ surgery cost?
In a less-specialised region you may have fewer experienced TMJ surgeons, meaning you might need to travel to a metropolitan centre (adding travel/lodging cost). You also may have fewer local follow-up therapy options, which may increase post-op cost/time. On the other hand, surgical fees in rural regions may be lower — but you must balance with quality of care and access. Ask about the surgeon’s volume of TMJ cases, outcome data, revision rates, and confirm follow-up therapy availability locally when planning.
Final Thoughts
In sum, when you ask “what is the TMJ surgery cost”, the answer is: it depends — and it can be significant. But with the right preparation, the right specialist and realistic expectations, the cost may well be an investment in long-term jaw joint health, reduced pain and enhanced quality of life. Your decision should be based on full understanding of the procedure, cost breakdown, alternatives, insurance coverage, recovery timeline and follow-up care. Armed with that knowledge, you can make an empowered choice about whether TMJ surgery is the right path for you.






